David
Ott
has
over
28
years
of
experience
in
the
healthcare
and
financial
services
industries.
David
has
provided
leadership
and
direction
to
department
leaders
and
teams
that
support
various
functions,
including
business
development,
payment
integrity,
claims
processing,
global
project
management
...
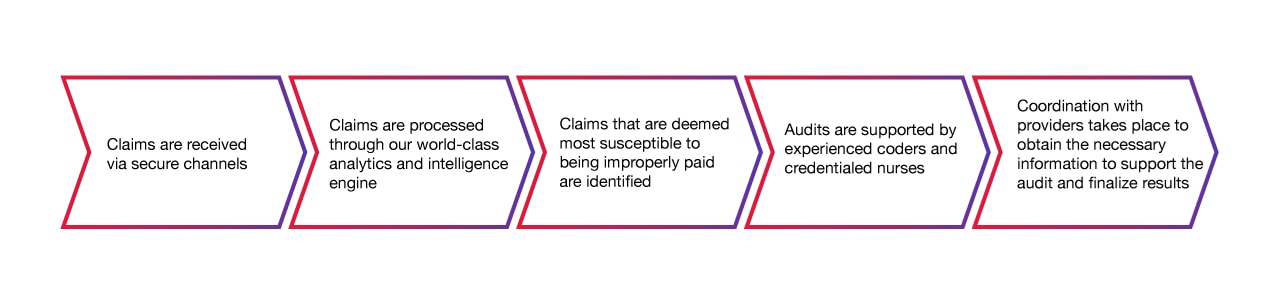
Enabling a robust claims integrity process
As a health payer / insurer, you need a robust claims integrity process that improves coding accuracy and minimizes healthcare provider abrasion. CGI sets the standard with an industry-leading 96% appeal-uphold rate.
We provide access and transparency of audit findings to you and your hospitals and providers to create a more robust claims integrity process. The relationships we build with you and your provider community not only reduce provider abrasion, but ultimately improve coding accuracy through partnership and education.
Increased scrutiny on improperly billed claims is a smart way to control your medical loss ratio. However, as providers exercise their appeal rights at record rates, you need a trusted partner to meet increasing appeal volumes and satisfy State-mandated independent reviewer requirements.
CGI’s team of physicians, clinicians, and certified coders can help address increasing volumes of appeals to help you keep your recovered dollars. With more than 30 years of recovery audit experience, we understand the appeal process and have developed a wealth of knowledge about trends in appeal results and ways to efficiently organize the process. Our team has developed an objective approach resulting in a high level of success against all provider types, including providers who contract with physician advisory organizations.
- Hospital inpatient
-
- Coding validation
- Clinical validation
- Short stay outliers
- Outlier charge review
- Medically necessary admission
- Discharge status validation
- Related readmission
- Avoidable readmission
- Hospital acquired condition review
- Hospital outpatient
-
- Canceled procedures
- Inappropriate modifier usage
- Medical necessity
- Policy compliance
- Device credit review
- Line-item charge review
- Trauma team and emergency room levels
- Observation hours
- Diagnostic/therapeutic radiology
- Professional providers
-
- Facility/professional mismatch
- Ambulance services
- Anesthesia billing
- Inappropriate modifier usage
- Durable medical equipment billing
- Evaluation and management review
- Policy compliance
- Medical necessity