In today's fast-paced world, the gap between promises and delivery can be a source of immense frustration, whether it's a company bungling an order or a government agency mishandling crucial benefits. Complaints are not just common; they are a call for change. Government agencies, tasked with delivering essential services, understand the gravity of these grievances and the need for effective resolution.
Responding to complaints is a key piece of good customer service. Behind the scenes, however, organizations need to do more than just solve customer problems one by one. By harnessing the power of data analysis, organizations can uncover deep insights into their operations, pinpointing areas ripe for process improvement, identifying training gaps, and spotlighting underperforming teams or individuals.
This is the essence of true complaint resolution: not merely addressing a single issue but revolutionizing processes, enhancing staff training, and integrating cutting-edge technologies to eradicate systemic flaws. Artificial intelligence, a rapidly maturing technology, has become a pivotal force in complaint resolution and the broader realm of business process reengineering.
Consider the Medicare and Medicaid programs, serving millions through a network of healthcare providers and insurers. The Centers for Medicare and Medicaid Services (CMS) is committed to delivering top-tier healthcare options to beneficiaries. Yet, with such expansive reach, some recipients inevitably encounter hurdles in their healthcare journey. While perfection may be elusive, continuous improvement is the key to minimizing disruptions and enhancing the overall experience.
Holding health plans accountable
Accountability is particularly paramount in the realm of healthcare. CMS leverages its Health Plan Management System (HPMS) to meticulously oversee the enrollment and compliance activities of Medicare Advantage and Medicare Part D programs. Picture HPMS as a comprehensive data hub where private health plan organizations submit crucial plan and bid information. To participate as a Medicare Advantage plan, these organizations must prove their ability to deliver the benefits promised—an ongoing commitment to excellence.
CMS's rigorous due diligence doesn't end with accepting a plan into the program. Health plans are subject to continuous compliance monitoring with a keen focus on complaint reporting. Plans plagued by an excessive number of complaints may face mandatory remediation activities or, in severe cases, risk losing their approved status. HPMS serves as the definitive repository for plan complaints, systematically categorizing, aggregating, and reporting on beneficiary grievances to meet legislative mandates. This process shines a spotlight on plan organizations, holding them accountable for their performance.
As the prime contractor for HPMS, CGI Federal is leading a groundbreaking initiative to develop an AI-powered pilot program focused on complaint management and analysis. This pioneering effort aims to demonstrate the transformative capabilities of AI, establishing a new benchmark for accountability and enhancement in healthcare plan management.
Building the pilot
While the analysis and resolution of complaints are crucial, automating these processes within HPMS has to date proven challenging. Currently, customer service representatives manually input data into spreadsheets and conduct analyses—a method that is both time-consuming and inefficient, offering limited insights.
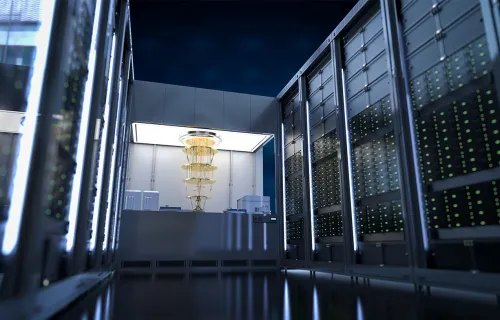
CGI is developing an AI-powered solution set to launch this November. This innovative solution is built on Amazon Web Services Agentic AI services, harnessing the power of large language models (LLMs) and natural language processing. Integrating an LLM, vector store and graph databases, the solution is designed to effectively identify patterns and trends, providing stakeholders with valuable insights into beneficiary issues. The aim is to aggregate, categorize, and analyze complaints swiftly, enabling faster reviews, trend identification, and enhanced CMS response to issues, thereby improving compliance monitoring.
Upon the solution’s completion, HPMS personnel will be able to analyze extensive data sets through a natural-language chat interface. This solution will exponentially accelerate the complaints review and analysis processes, quickly pinpointing top trends and reducing manual processing. It will empower users to identify plans with disproportionate complaint numbers, guiding leaders on necessary corrective measures.
Additionally, the system will facilitate AI-assisted sentiment analysis, allowing for the tracking of public perception and the identification of emerging trends that may impact multiple insurers within the program. This will lead to more effective resolution, mitigation, and reporting, ultimately enhancing beneficiary satisfaction.
AI tools offer tremendous potential for deeper data exploration with unprecedented efficiency. While the tools have limitations, CGI understands the challenges and is helping CMS to avoid pitfalls. Staff training and education and emphasizing the importance of human validation are integral to adopting and operationalizing AI and these are important elements of our solution. Our work at CMS is set to create a more cost-effective program, delivering superior service levels to beneficiaries in the near future.
Learn more about our work in the federal healthcare sector, visit our website. Also, check out what we are optimizing AI for Federal agencies.